The school nurse called me about three kindergarteners with crusty sores around their mouths. “We’ve got impetigo again,” she sighed. “Every year it’s the same story.”
She’s right. Schools create perfect conditions for impetigo spread, making this bacterial skin infection a recurring nightmare for parents, teachers, and healthcare providers alike.
What Makes Schools High-Risk
Close contact among children facilitates easy transmission. Kids touch each other constantly during play, sports, and daily interactions.
Shared surfaces like desks, playground equipment, and bathroom facilities harbor bacteria that can survive for hours.
Poor hand hygiene among young children means they frequently touch contaminated surfaces then touch their faces, creating infection opportunities.
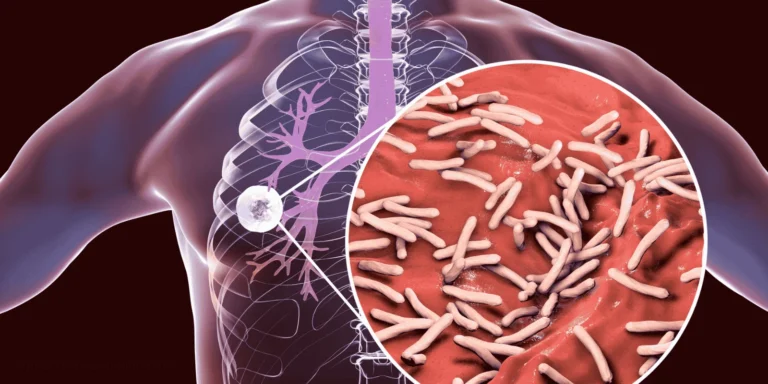
How Impetigo Spreads
Direct skin contact with infected sores transmits bacteria most efficiently. Even brief contact during play can transfer enough bacteria to start new infections.
Contaminated objects like toys, towels, clothing, or sports equipment can carry bacteria between children.
Scratching behavior common in kids helps spread infection to new body areas and contaminates fingernails, which then touch other children or surfaces.
Age Factors in School Spread
Younger children (ages 2-5) have the highest impetigo rates due to developing immune systems and hygiene habits.
Elementary students still struggle with consistent handwashing and tend to touch their faces frequently.
Close-contact activities like wrestling, soccer, or playground games in any age group increase transmission risk.
Why Some Kids Get It Repeatedly
Carriers without symptoms can harbor bacteria on their skin and spread infection without appearing ill themselves.
Incomplete treatment allows bacteria to persist and reinfect the same child or spread to others.
Skin conditions like eczema create breaks in the skin barrier, making certain children more susceptible to repeated infections.
Seasonal Patterns in Schools
Late summer/early fall sees peak impetigo rates as children return to close school contact after summer activities that may have caused minor skin injuries.
Post-holiday spikes occur after breaks when children return from various family activities and exposures.
Warm weather months promote bacterial growth and increase minor cuts and scrapes that provide entry points.
Recognition in School Settings
Honey-crusted lesions around the mouth, nose, or hands are classic impetigo signs teachers learn to identify.
Multiple children affected in the same classroom or grade level suggests ongoing transmission.
Scratching behavior in affected children can indicate spreading infection before obvious sores appear.
School Response Protocols
Exclusion policies typically require children to stay home until 24 hours after starting antibiotic treatment.
Cleaning procedures focus on disinfecting shared surfaces, toys, and equipment that may harbor bacteria.
Parent notification alerts families to watch for symptoms in their children and seek prompt treatment.
Why Early Treatment Matters
Bacterial multiplication accelerates in school environments where reinfection opportunities abound.
Spread prevention requires treating infected children quickly to reduce bacterial shedding.
Complication avoidance becomes important when multiple children are affected, as untreated impetigo can lead to deeper skin infections.
Treatment Considerations for School Cases
Topical antibiotics work well for localized infections but require consistent application that may be challenging during school hours.
Oral antibiotics might be preferred for school-age children to ensure consistent treatment and faster return to school.
Wound care education helps children and families prevent spread to other body areas or family members.
Prevention Strategies
Hand hygiene education focusing on proper technique and frequency, especially before eating and after playground time.
Don’t share personal items like towels, clothing, or sports equipment that can transfer bacteria.
Prompt wound care for cuts, scrapes, or insect bites prevents bacterial entry through damaged skin.
Clean sports equipment and shared toys regularly with appropriate disinfectants.
When to Keep Kids Home
Active, uncovered lesions pose high transmission risk and require exclusion until treated.
First 24 hours of antibiotic treatment allow time for bacterial reduction before safe school return.
Fever or systemic illness accompanying impetigo suggests more serious infection requiring extended recovery time.
Parent Education Points
Recognition skills help parents identify impetigo early before significant spread occurs.
Treatment compliance ensures complete bacterial elimination and prevents reinfection or complications.
Communication with school allows coordination of prevention efforts and appropriate return timing.
Schools will continue seeing impetigo outbreaks due to the nature of childhood social interaction. However, understanding transmission patterns, implementing consistent prevention measures, and ensuring prompt treatment can significantly reduce outbreak severity and duration.