“Half my wrestling team has jock itch,” a high school coach told me. “Why does this keep happening?”
Athletic activities create perfect conditions for fungal infections like jock itch to develop and spread. Understanding these risk factors helps athletes prevent this uncomfortable and embarrassing condition.
Why Athletes Are Prime Targets
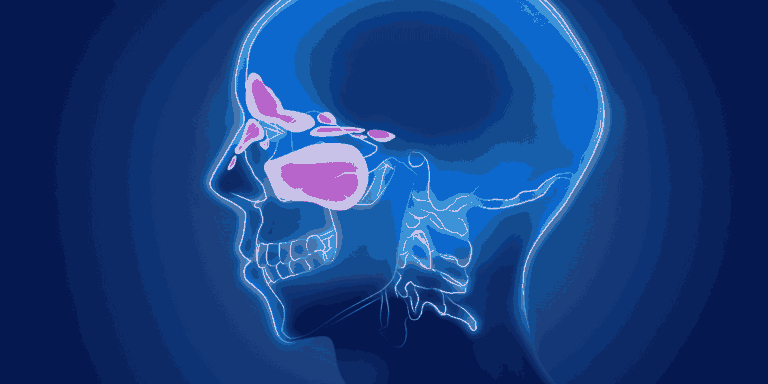
Excessive sweating during training and competition creates the warm, moist environment that fungi need to thrive.
Tight athletic gear traps moisture against skin, preventing evaporation and maintaining ideal fungal growth conditions.
Friction from movement damages skin’s protective barrier, creating entry points for fungal invasion.
Prolonged moisture exposure during extended practices or competitions prevents skin from drying between activities.
High-Risk Sports
Wrestling involves close body contact, shared mats, and heavy sweating in tight clothing.
Football requires wearing equipment that traps heat and moisture for extended periods.
Running creates repetitive friction in the groin area combined with profuse sweating.
Cycling produces sustained pressure and friction in the groin region while wearing tight, moisture-trapping clothing.
Swimming exposes athletes to warm, humid locker room environments where fungi flourish.
Locker Room Environment
Shared facilities allow fungal transmission through contaminated benches, floors, and equipment.
Warm, humid conditions in locker rooms and showers provide ideal fungal growth environments.
Communal equipment like towels, athletic supporters, or shared clothing can spread infections.
Poor ventilation prevents moisture from dissipating, maintaining conditions that support fungal survival.
Athletic Clothing Factors
Synthetic fabrics without moisture-wicking properties trap sweat against skin.
Tight-fitting gear reduces airflow and increases friction that damages protective skin barriers.
Multiple-hour wear during practices, games, and travel prevents skin from breathing and drying.
Delayed changing after sweating allows prolonged fungal exposure to vulnerable skin.
Body Contact Sports Risks
Skin-to-skin contact can transfer fungi directly between athletes during competition or practice.
Mat and equipment sharing in sports like wrestling, martial arts, or gymnastics spreads fungal contamination.
Shared protective gear that contacts the groin area can harbor and transmit fungi.
Why Reinfection Happens
Contaminated equipment continues exposing athletes even after successful treatment.
Team spread means treating one athlete doesn’t prevent reinfection from untreated teammates.
Environmental reservoirs in locker rooms and training facilities maintain ongoing exposure.
Incomplete treatment allows fungi to persist and quickly reestablish infection.
Prevention Strategies
Moisture management through frequent clothing changes and thorough drying after activities.
Breathable fabrics that wick moisture away from skin reduce fungal growth conditions.
Antifungal powder applied before activities helps keep the groin area dry and inhibits fungal growth.
Immediate showering after practices or competitions removes sweat and reduces fungal exposure time.
Equipment and Facility Hygiene
Regular mat cleaning with antifungal disinfectants in contact sports.
Personal equipment for items that touch the groin area rather than sharing gear.
Locker room maintenance including ventilation improvements and regular disinfection.
Clean towels for each use rather than reusing damp towels that harbor fungi.
Early Recognition Benefits
Mild itching and slight redness respond faster to treatment than advanced infections.
Prompt treatment prevents spread to teammates and reduces contagious period.
Self-awareness helps athletes identify problems before they become severe or widespread.
Treatment Considerations for Athletes
Continue competition may be possible with appropriate antifungal treatment and coverage.
Contagion concerns require isolation from contact sports until treatment begins showing results.
Multiple treatment locations — treat feet if athlete’s foot is present to prevent reinfection.
Extended treatment courses may be needed given ongoing exposure to risk factors.
Team Management
Education programs about prevention reduce overall team infection rates.
Screening protocols help identify and treat cases before widespread transmission.
Environmental interventions in training facilities reduce fungal contamination.
Treatment compliance monitoring ensures athletes complete full medication courses.
Long-Term Prevention
Habit formation around immediate changing and showering after activities.
Equipment inspection and regular replacement of worn or contaminated gear.
Facility improvements addressing ventilation and moisture control in locker areas.
Ongoing vigilance since athletic environments will always pose elevated fungal infection risks.
Athletes’ increased jock itch risk stems from unavoidable aspects of training and competition, but understanding these factors enables effective prevention strategies that reduce infection rates without compromising athletic performance.