“My daughter can’t have ringworm,” a mother insisted during our consultation. “We don’t have any worms in our house, and she takes baths every day.”
Despite being one of the most common fungal infections, ringworm remains surrounded by misconceptions that delay proper treatment and prevention efforts.
Myth #1: Ringworm Is Caused by Worms
Reality: Ringworm is a fungal infection with no worms involved. The name comes from the circular, ring-like appearance of the rash.
The fungi responsible belong to a group called dermatophytes that specifically target skin, hair, and nails.
Historical naming occurred before microscopes allowed doctors to identify the true fungal cause of these distinctive circular rashes.
Myth #2: Only Dirty People Get Ringworm
Reality: Excellent hygiene doesn’t prevent ringworm infection. The fungi are extremely common in environments and can affect anyone.
Clean, healthy skin can still develop ringworm after exposure to contaminated surfaces, animals, or infected people.
Athletes frequently develop ringworm despite excellent hygiene practices, particularly in areas like feet (athlete’s foot) and groin (jock itch).
Myth #3: Ringworm Only Affects Children
Reality: All age groups can develop ringworm, though children may have more exposure opportunities in schools and daycare settings.
Adults commonly develop athlete’s foot and jock itch, both forms of ringworm affecting different body areas.
Elderly individuals may be more susceptible due to weakened immune systems or circulation problems.
Myth #4: You Can’t Catch Ringworm from Pets
Reality: Animals are major sources of human ringworm infections, particularly cats, dogs, and farm animals.
Pet transmission often occurs through direct contact or contaminated bedding, toys, and grooming supplies.
Asymptomatic pets can carry and spread ringworm fungi without showing visible signs of infection themselves.
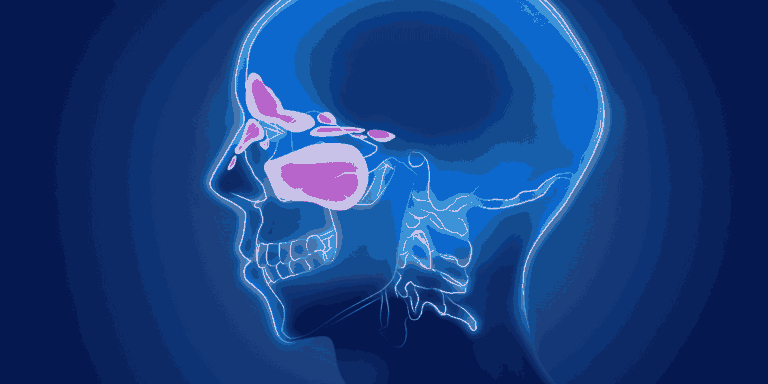
Myth #5: Ringworm Always Forms Perfect Circles
Reality: While classic ringworm creates circular patches with clear centers, many infections don’t follow this pattern.
Scalp ringworm often appears as scaly patches with hair loss rather than distinct rings.
Facial ringworm may look like eczema or other skin conditions without obvious circular borders.
Multiple lesions can merge together, creating irregular shapes that don’t resemble rings at all.
Myth #6: Ringworm Is Highly Contagious
Reality: While ringworm can spread between people, transmission requires direct contact or sharing contaminated items.
Casual contact like being in the same room doesn’t typically spread the infection.
Personal items like towels, clothing, and hairbrushes pose higher transmission risk than airborne spread.
Myth #7: Over-the-Counter Treatments Don’t Work
Reality: Most ringworm infections respond well to topical antifungal creams available without prescription.
Early treatment with OTC medications often eliminates infections within 2-4 weeks.
Prescription medications become necessary for severe infections, scalp involvement, or treatment failures.
Myth #8: Bleach Kills Ringworm on Surfaces
Reality: While bleach has some antifungal properties, it’s not the most effective disinfectant for ringworm fungi.
Better options include antifungal sprays specifically designed for surface disinfection.
Hot water washing (140°F or higher) effectively kills ringworm spores on clothing and bedding.
Myth #9: Ringworm Scars Are Permanent
Reality: Most ringworm infections heal without leaving permanent marks when treated appropriately.
Temporary discoloration may persist for weeks to months after infection clears but usually fades completely.
Scarring only occurs with severe infections that aren’t treated promptly or become secondarily infected with bacteria.
Myth #10: Natural Remedies Work as Well as Medicine
Reality: While some natural substances have antifungal properties, proven medical treatments are more reliable and faster-acting.
Tea tree oil and other natural remedies may help but shouldn’t replace proven antifungal medications.
Delayed effective treatment allows infections to spread and become more difficult to eliminate.
Prevention Facts vs. Fiction
Regular bathing helps but doesn’t guarantee prevention since fungi can survive on skin temporarily before establishing infection.
Avoid sharing personal items like towels, clothing, and grooming supplies, especially in gyms or sports facilities.
Dry skin thoroughly after bathing, particularly in warm, moist areas where fungi thrive.
Pet hygiene includes regular veterinary care to identify and treat fungal infections in animals.
Treatment Reality Check
Complete treatment courses are essential even after visible symptoms disappear, as fungi may persist in skin layers.
All affected areas require treatment, including areas that don’t show obvious symptoms but may harbor infection.
Follow-up evaluation helps ensure complete elimination and prevents recurrence from incomplete treatment.
Understanding the facts about ringworm helps people take appropriate prevention measures and seek effective treatment without unnecessary fear or delay.