“Is this the beginning of shingles or just a bug bite?” my patient asked, pointing to a small red area on her side. “How can I tell?”
Shingles progresses through distinct stages with characteristic appearances that help identify the condition and determine appropriate treatment timing.
Pre-Rash Stage (Days 1-5)
Pain precedes visible rash by several days in most cases, often described as burning, tingling, or stabbing sensations.
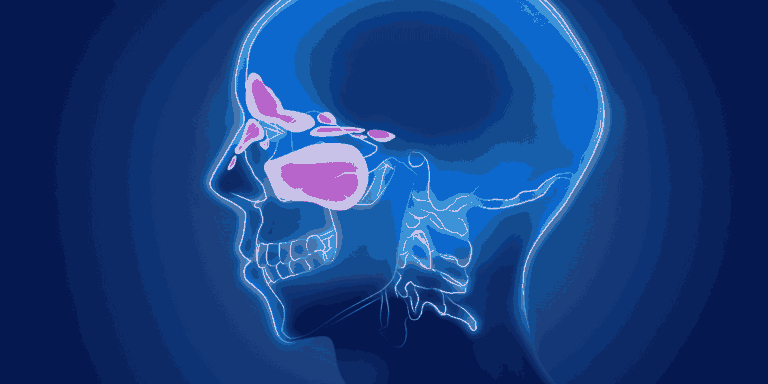
Location-specific discomfort follows nerve pathways, typically affecting one side of the body or face.
Flu-like symptoms including fatigue, headache, and sensitivity to light may occur without visible skin changes.
Skin sensitivity in the affected area makes clothing or light touch uncomfortable.
Early Rash Stage (Days 5-7)
Red patches appear in the painful area, initially looking like clusters of red bumps or hives.
Unilateral distribution — rash stops sharply at the body’s midline, affecting only one side.
Band or belt-like pattern follows specific nerve distribution areas called dermatomes.
Itching begins as the immune system responds to virus reactivation in nerve endings.
Blister Stage (Days 7-10)
Fluid-filled blisters develop on the red patches, resembling chickenpox but in a more confined, linear pattern.
Clear fluid content initially fills the blisters, which are the most contagious stage.
Grouping pattern shows clusters of blisters close together along nerve pathways.
Pain intensifies as inflammation peaks and nerve involvement becomes maximal.
Weeping Stage (Days 10-12)
Blisters rupture releasing clear or slightly cloudy fluid that can spread virus to susceptible people.
Raw, moist areas appear where blisters have broken, looking similar to minor burns.
Highest contagion risk occurs during this phase when virus-containing fluid is exposed.
Infection vulnerability increases as broken skin creates entry points for bacteria.
Crusting Stage (Days 12-14)
Scabs form over ruptured blisters as the body begins healing process.
Dried, crusty appearance replaces the moist, weeping stage.
Reduced contagiousness begins as virus becomes contained under forming scabs.
Pain may persist even as visible healing progresses.
Healing Stage (Weeks 2-4)
Scabs fall off gradually, revealing new pink skin underneath.
No longer contagious once all blisters have completely crusted over.
Skin discoloration may persist for weeks or months after lesions heal.
Scarring is uncommon unless blisters became infected or were scratched excessively.
Post-Healing Phase (Months After)
Post-herpetic neuralgia can cause persistent nerve pain in previously affected areas.
Skin sensitivity may remain in healed areas for extended periods.
Pigment changes gradually fade but can take 6-12 months to completely resolve.
Unusual Presentations
Disseminated shingles affects multiple body areas and appears more like chickenpox, seen mainly in immunocompromised patients.
Shingles without rash (zoster sine herpete) causes nerve pain without visible skin lesions.
Facial shingles affecting the eye area requires immediate treatment to prevent vision complications.
When to Seek Treatment
Within 72 hours of rash appearance for antiviral medications that reduce severity and duration.
Eye involvement requires immediate ophthalmologic evaluation to prevent corneal damage.
Severe pain may need prescription pain management beyond over-the-counter options.
Signs of bacterial infection including increasing redness, swelling, or pus formation.
Treatment Impact on Stages
Early antiviral treatment can reduce rash severity, shorten duration, and decrease post-herpetic neuralgia risk.
Pain management throughout all stages improves comfort and prevents chronic pain development.
Proper wound care during weeping and crusting stages prevents bacterial superinfection.
Preventing Spread
Cover all lesions completely until fully crusted over to prevent transmission.
Avoid contact with pregnant women, newborns, and immunocompromised individuals during contagious phases.
Hand hygiene after touching affected areas prevents spreading virus to other body parts or people.
Complications to Monitor
Secondary bacterial infection shows increasing redness, warmth, swelling, or pus.
Dissemination with new lesions appearing in distant body areas requires immediate medical attention.
Neurological symptoms like weakness or numbness beyond the rash area need urgent evaluation.
Long-Term Outlook
Complete healing typically occurs within 4-6 weeks for most people.
Post-herpetic neuralgia risk increases with age, affecting up to 20% of patients over 60.
Recurrence is uncommon but possible, with most people experiencing only one shingles episode.
Understanding shingles progression helps you recognize the condition early when treatment is most effective and allows for appropriate precautions during contagious phases.