“The urgent care doctor wouldn’t prescribe antibiotics after I pulled off a tick,” my patient complained. “Don’t I need protection against Lyme disease?”
Doctors follow specific evidence-based guidelines for tick bite prophylaxis that prevent overuse of antibiotics while protecting people at genuine risk. Understanding these criteria helps set realistic expectations.
The Core Guideline Requirements
All five criteria must be met for prophylactic antibiotic recommendation:
- Identified blacklegged (deer) tick
- Estimated attachment 36+ hours
- Removed within 72 hours
- High-risk geographic area (>20% infection rate)
- No contraindications to doxycycline
Missing even one criterion means prophylaxis isn’t recommended based on current evidence.
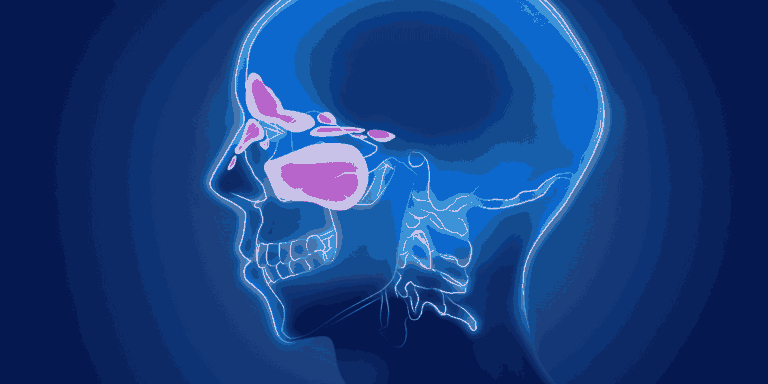
Why the 36-Hour Rule Exists
Disease transmission timing — Lyme bacteria need time to migrate from tick gut to salivary glands and into the human host.
Research evidence consistently shows minimal transmission occurs before 36 hours of attachment.
Tick engorgement helps estimate attachment duration — flat ticks haven’t fed long enough for disease transmission.
Geographic Risk Assessment
High-risk areas include northeastern states, upper Midwest, and northern California where Lyme disease is endemic.
Local data guides decisions since risk varies significantly even within states or regions.
Travel history matters — where the tick bite occurred determines geographic risk, not where you live.
Tick Species Identification
Blacklegged ticks (deer ticks) are the only species that transmit Lyme disease bacteria.
Size matters — these ticks are tiny, about the size of a poppy seed when unfed.
Other tick species like dog ticks, lone star ticks, or American wood ticks don’t carry Lyme disease regardless of attachment duration.
The 72-Hour Window
Treatment effectiveness decreases significantly if started more than 72 hours after tick removal.
Single-dose doxycycline (200mg) is the recommended prophylaxis when criteria are met.
Timing calculation starts from tick removal, not from when the bite occurred.
Why Not Treat Everyone
Side effects from doxycycline include nausea, sun sensitivity, and rare but serious allergic reactions.
Antibiotic resistance concerns make unnecessary antibiotic use problematic for public health.
Low absolute risk — even in high-risk areas with long-attached ticks, infection risk is typically under 5%.
Treatment availability if infection develops — early Lyme disease responds excellently to standard antibiotic courses.
Special Population Considerations
Children under 8 shouldn’t receive doxycycline due to tooth discoloration risks.
Pregnant women require alternative approaches since doxycycline affects fetal bone and tooth development.
Drug allergies or interactions may preclude standard prophylaxis even when otherwise indicated.
Watchful Waiting Alternative
Most doctors recommend monitoring for symptoms rather than routine prophylaxis for bites not meeting all criteria.
Symptom awareness education about erythema migrans rash and flu-like symptoms allows early treatment if infection develops.
Follow-up access ensures patients can return quickly if concerning symptoms appear.
What Patients Should Monitor
Expanding rash developing 3-30 days after tick bite, especially if it reaches 2+ inches in diameter.
Flu-like symptoms including fever, headache, muscle aches, and fatigue.
Multiple lesions — Lyme disease can cause secondary rash spots distant from the original bite.
Joint pain or neurological symptoms developing weeks after tick exposure.
Why Some Doctors Vary
Clinical judgment allows consideration of individual risk factors beyond standard guidelines.
Patient anxiety sometimes influences decisions, though guidelines don’t support this as a primary factor.
Local practice patterns may differ based on regional Lyme disease prevalence and experience.
International Guideline Differences
European guidelines differ from American recommendations regarding prophylaxis indications.
Canadian approaches vary by province based on local tick populations and disease prevalence.
Evidence interpretation leads to some legitimate medical disagreement about optimal approaches.
Cost-Effectiveness Considerations
Single-dose prophylaxis is inexpensive but must be weighed against treatment of the few infections that would develop.
Resource allocation affects public health recommendations about widespread prophylaxis use.
Insurance coverage varies for prophylactic versus therapeutic antibiotic prescriptions.
Documentation Importance
Save the tick when possible for identification if symptoms develop later.
Photo evidence of the tick and bite site helps later assessment if concerns arise.
Record details including removal date, location of exposure, and attachment duration estimates.
Patient Education Priority
Symptom recognition trumps prophylaxis — knowing what to watch for enables early treatment.
Realistic risk assessment prevents unnecessary anxiety while maintaining appropriate vigilance.
Follow-up plan ensures patients know when and how to seek care if problems develop.
Understanding these guidelines helps patients recognize that physicians refusing prophylaxis aren’t being dismissive but rather following evidence-based protocols that balance individual protection with broader antibiotic stewardship concerns.