You blow your nose and see thick green mucus. You immediately think, “I need antibiotics.” But here’s what surprises most people: green or yellow mucus doesn’t automatically mean bacterial infection. Through ChatRx’s chat-based e-visits, I regularly tell patients with colored mucus they don’t need antibiotics, and here’s why.
Let me explain what actually determines whether antibiotics help versus waste your money.
Why Mucus Turns Colors
Your immune system produces white blood cells to fight infections, whether viral or bacterial. When these white blood cells die, they release enzymes that turn mucus yellow or green.
This color change happens with ANY infection your body is fighting. Viral colds cause colored mucus. Bacterial sinus infections cause colored mucus. The color alone doesn’t distinguish between them.
I’ve seen patients suffer from viral infections with bright green mucus who didn’t need antibiotics, and patients with bacterial sinusitis with clear mucus who did need treatment. Color is just one piece of the puzzle.
What ChatRx Actually Evaluates
Use the free symptom checker first to provide your symptom pattern. In about 2 minutes, it analyzes multiple factors beyond mucus color.
Through the full e-visit for $25, I look at symptom duration. How long have you been sick? Viral infections typically improve after 7 to 10 days. Symptoms persisting beyond 10 days without improvement suggest bacterial infection worth treating.
The “double worsening” pattern matters more than color. You start improving from a cold, then suddenly get worse again. This suggests bacteria took advantage while your defenses were down.
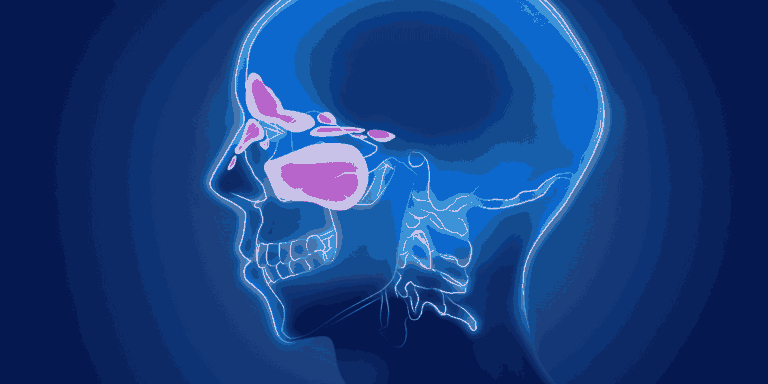
Severity and Location
Facial pain severity and location provide better clues than mucus color. Deep, aching pain in your cheeks or forehead that worsens when bending forward suggests bacterial sinusitis.
Mild congestion and pressure, even with green mucus, usually indicates viral infection still resolving. Your body is doing its job fighting the virus. Give it time.
Fever Patterns
Persistent fever or fever developing after initial improvement points toward bacterial infection more reliably than mucus color.
Low-grade fever for a day or two during a cold is normal. Fever above 101 degrees lasting several days warrants antibiotic consideration regardless of mucus appearance.
Associated Symptoms
Tooth pain or bad breath along with green mucus suggests bacterial sinusitis. These symptoms indicate infection in your upper sinuses near teeth.
Just feeling crummy with congestion and colored mucus? Probably still viral. Most people with colds produce colored mucus for a few days as the infection peaks.
The Timeline Test
Green mucus on day 3 of a cold? Almost certainly viral. Your immune system is actively fighting, producing that color change.
Green mucus on day 14 with no improvement? More likely bacterial, though color isn’t the deciding factor. The duration and lack of improvement drive the antibiotic decision.
What Studies Show
Research confirms colored mucus alone doesn’t predict who benefits from antibiotics. Doctors who prescribe based on color alone are overtreating viral infections.
The clinical guidelines I follow through ChatRx focus on symptom duration, severity, and pattern rather than mucus appearance.
When I Prescribe Antibiotics
Symptoms lasting more than 10 days without improvement get antibiotics, regardless of mucus color. The duration tells me your immune system needs help.
Severe symptoms from the start with high fever, intense facial pain, and very thick discharge warrant antibiotics even earlier.
The double worsening pattern. Clear worsening after initial improvement suggests bacterial superinfection.
When I don’t Prescribe Antibiotics
Colored mucus for less than 10 days in someone steadily improving? No antibiotics. You’re recovering normally from a viral infection.
Mild symptoms even with green mucus that are slowly getting better? No antibiotics. Time and symptom management will resolve this.
Green mucus without other concerning features like high fever, severe pain, or prolonged duration? No antibiotics. Color alone doesn’t justify treatment.
What You Get Instead
For viral infections with colored mucus, I provide comprehensive symptom management guidance. Saline rinses help clear thick mucus. Decongestants reduce pressure. Pain relievers ease discomfort.
Most patients feel significantly better within days using these strategies, without antibiotics and their potential side effects.
The Bottom Line
Stop assuming green mucus means you need antibiotics. Use ChatRx’s free symptom checker to evaluate your complete symptom pattern. If the full e-visit assessment indicates viral infection, save money and avoid unnecessary antibiotics. If bacterial infection seems likely based on proper criteria, you’ll get appropriate treatment fast.