“My neighbor got antibiotics for her bronchitis last month,” my patient told me. “Why won’t you prescribe them for me?”
This conversation happens in my office almost daily, especially during cold and flu season. The truth about antibiotics and bronchitis might surprise you — and understanding when they help versus when they harm can make the difference between faster healing and prolonged illness.
The Antibiotic Reality Check
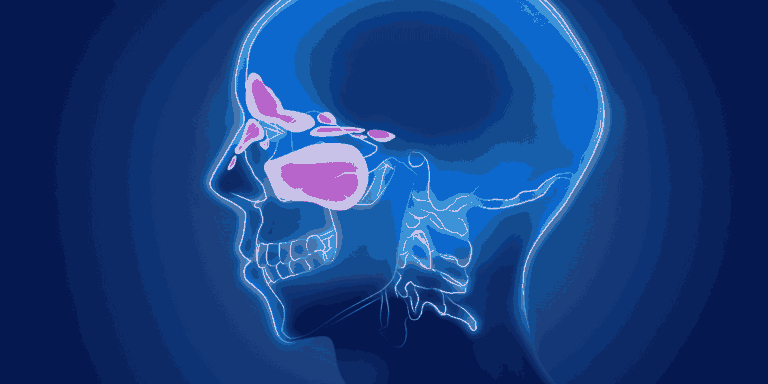
Here’s the fundamental issue: most acute bronchitis is caused by viruses, not bacteria. Antibiotics kill bacteria but have zero effect on viruses. Taking antibiotics for viral bronchitis is like using a screwdriver to hammer a nail — it’s the wrong tool for the job.
Research consistently shows that 90-95% of acute bronchitis cases in healthy adults are viral. This means antibiotics provide no benefit for the vast majority of patients, while potentially causing harm through side effects and antibiotic resistance.
When Antibiotics Help
The small percentage of bronchitis cases that benefit from antibiotics typically involve:
Secondary bacterial infections that develop after initial viral bronchitis. Signs include worsening symptoms after initial improvement, high persistent fever, and significantly thickened, colored sputum.
Patients with chronic lung conditions like COPD, where bacterial infections are more common and potentially more serious.
Immunocompromised individuals who face higher risk of bacterial complications from initial viral infections.
Suspected pneumonia rather than simple bronchitis, which requires different evaluation and treatment approaches.
The Dangers of Unnecessary Antibiotics
Taking antibiotics when you don’t need them isn’t harmless. Real risks include:
Antibiotic resistance develops when bacteria adapt to survive antibiotic exposure. Each unnecessary course increases the chance that future bacterial infections won’t respond to standard treatments.
Disrupted gut bacteria can cause digestive problems, increase infection risk elsewhere in your body, and take weeks or months to recover normal balance.
Allergic reactions range from mild rashes to life-threatening anaphylaxis. Every antibiotic exposure carries this risk, making unnecessary use particularly problematic.
C. diff infections can develop when antibiotics kill beneficial gut bacteria, allowing dangerous C. difficile bacteria to overgrow and cause severe, sometimes fatal colitis.
Drug interactions become more likely as you add antibiotics to other medications you might be taking.
Why the Confusion Exists
Several factors contribute to antibiotic overuse in bronchitis:
Patient expectations often include wanting “something” to treat symptoms, and antibiotics feel like active treatment compared to supportive care.
Symptom severity can make viral bronchitis feel serious enough to warrant antibiotic treatment, even when it won’t help.
Colored sputum misleads many people into thinking bacterial infection is present, but viruses commonly cause yellow or green mucus too.
Previous experiences where people felt better after taking antibiotics for respiratory infections may create false associations between antibiotics and recovery.
What Helps Viral Bronchitis
Instead of antibiotics, focus on treatments that actually address viral bronchitis:
Rest and hydration support your immune system’s ability to fight the viral infection effectively.
Cough suppressants can provide nighttime relief when coughing disrupts sleep, though productive coughs during the day help clear infected material.
Expectorants like guaifenesin help thin mucus, making it easier to cough up and clear from your airways.
Steam inhalation soothes irritated airways and helps loosen secretions naturally.
Pain relievers like acetaminophen or ibuprofen reduce fever and body aches while your immune system works.
Honey has natural anti-inflammatory properties and can soothe throat irritation and reduce cough frequency.
Recognizing When You Might Need Antibiotics
Contact your healthcare provider if you develop:
High fever (over 101°F) that persists beyond the first week or returns after initial improvement.
Shortness of breath at rest or with minimal activity, which might indicate pneumonia rather than simple bronchitis.
Worsening symptoms after 7-10 days, especially if accompanied by fever and significantly increased sputum production.
Blood in sputum that’s more than occasional streaking from vigorous coughing.
Signs of pneumonia including sharp chest pain that worsens with breathing, severe fatigue, or feeling much sicker than typical bronchitis.
The Responsible Prescribing Approach
When I evaluate patients with bronchitis, I consider several factors:
Symptom duration and pattern help distinguish viral from bacterial causes.
Overall health status influences infection risk and complications potential.
Physical examination findings can reveal signs of pneumonia or other complications.
Risk factors like COPD, heart disease, or immune system problems affect treatment decisions.
Patient Safety and Antibiotic Stewardship
As healthcare providers, we balance individual patient needs with broader public health concerns:
Individual safety means avoiding unnecessary medication risks while ensuring appropriate treatment when needed.
Community protection involves preserving antibiotic effectiveness for future patients who will genuinely need these medications.
Evidence-based decisions rely on medical research rather than patient pressure or provider convenience.
What to Expect With Viral Bronchitis
Understanding the natural course helps set realistic expectations:
Symptoms typically peak around days 4-7, then gradually improve over 2-3 weeks.
Cough may persist for 4-8 weeks as airway inflammation slowly resolves.
Energy levels usually return to normal within 1-2 weeks, though some fatigue may linger.
Complete recovery occurs in nearly all healthy adults with supportive care alone.
Making Informed Decisions Together
The best medical decisions happen when patients and providers work together with accurate information:
Discuss your concerns openly with your healthcare provider about symptom severity and recovery expectations.
Understand the reasoning behind treatment recommendations, whether they include antibiotics or focus on supportive care.
Ask questions about warning signs that would indicate need for antibiotic treatment or further evaluation.
The Long-Term Perspective
Every antibiotic decision affects not just your immediate health, but also contributes to larger patterns of antibiotic resistance that impact entire communities.
Responsible use means taking antibiotics only when they’re truly needed and always completing the full prescribed course.
Prevention focus emphasizes vaccination, good hygiene, and lifestyle factors that reduce infection risk overall.
The Bottom Line
Antibiotics are generally not safe or effective for most cases of acute bronchitis because the condition is usually viral. Taking them unnecessarily exposes you to real risks including allergic reactions, digestive problems, and contributing to antibiotic resistance.
However, certain high-risk situations and bacterial complications do warrant antibiotic treatment. The key is accurate diagnosis and individualized decision-making based on your specific symptoms, health status, and risk factors.
Focus on proven supportive treatments for viral bronchitis, and trust that your immune system can handle most respiratory infections with proper rest and care. Save antibiotics for the bacterial infections where they can truly make a difference.