“This is my daughter’s fourth ear infection this year,” an exhausted mother told me. “Why does this keep happening?”
Some children seem stuck in an endless cycle of ear infections, frustrating families and raising questions about underlying causes. Understanding why certain kids experience repeated episodes helps break the pattern.
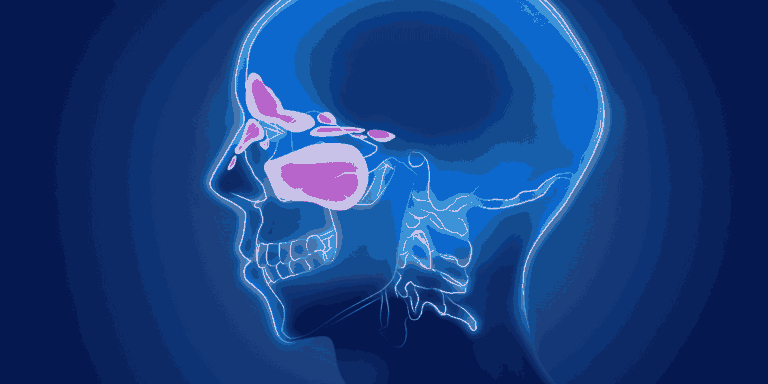
Anatomy Creates Vulnerability
Eustachian tube structure in young children makes them prone to ear problems. These tubes are shorter, more horizontal, and narrower than in adults.
Poor drainage results when eustachian tubes can’t effectively clear fluid from the middle ear space, creating breeding grounds for bacteria.
Tube immaturity means the normal opening and closing mechanism doesn’t work properly, allowing bacteria to travel from the throat to the ear.
Age-Related Risk Patterns
Peak occurrence happens between 6 months and 3 years when eustachian tubes are most immature and immune systems are still developing.
Gradual improvement typically occurs as children grow and their anatomy matures, usually by ages 4-6.
Individual variation means some children outgrow the tendency earlier while others continue having problems into school age.
Environmental Triggers
Daycare exposure dramatically increases infection risk due to constant cold virus circulation among children in close contact.
Secondhand smoke irritates respiratory passages and impairs the body’s ability to clear bacteria from the ear and throat.
Seasonal allergies cause inflammation that blocks eustachian tubes, preventing normal drainage and creating infection-prone conditions.
Upper respiratory infections like colds create swelling that blocks ear drainage, often leading to secondary bacterial infections.
Underlying Medical Factors
Adenoid enlargement can block eustachian tube openings, preventing proper ear ventilation and drainage.
Cleft palate or other anatomical variations affect muscle function needed for normal eustachian tube operation.
Immune deficiencies make some children less able to fight off bacterial infections once they establish in the middle ear.
Gastroesophageal reflux can irritate the throat and eustachian tubes, contributing to inflammation and blockage.
The Cycle Effect
Incomplete healing from previous infections can leave residual fluid that becomes reinfected with new bacterial exposure.
Scar tissue formation may interfere with normal eustachian tube function, creating permanent drainage problems.
Antibiotic resistance develops when repeated courses create bacterial strains that don’t respond to standard treatments.
Prevention Strategies
Reduce cold exposure by limiting daycare during peak illness seasons when possible, though this isn’t practical for many families.
Breastfeeding provides immune protection and reduces infection risk, especially important during the first year.
Avoid bottle propping which allows formula to pool in the throat area and potentially reach the eustachian tubes.
Control allergies with appropriate medications during seasons when environmental triggers are highest.
Eliminate smoke exposure completely, as even minimal exposure increases ear infection risk significantly.
When Medical Intervention Helps
Ear tubes (tympanostomy tubes) provide artificial drainage when natural eustachian tube function is inadequate.
Adenoidectomy may help when enlarged adenoids block eustachian tube openings.
Prophylactic antibiotics are occasionally used during high-risk periods, though this approach is controversial.
Hearing evaluation ensures repeated infections aren’t causing permanent hearing loss that could affect development.
Signs It’s Time for Specialist Care
More than 4-6 infections per year suggests underlying issues that may benefit from ENT evaluation.
Hearing concerns including delayed speech development or not responding to sounds appropriately.
Persistent fluid behind eardrums that doesn’t clear between infection episodes.
Treatment failures where standard antibiotics consistently fail to clear infections.
Long-Term Outlook
Most children outgrow the tendency for recurrent ear infections as their anatomy matures and immune systems strengthen.
Complications are rare when infections receive appropriate treatment, though hearing monitoring remains important.
Speech and development typically remain normal unless hearing loss becomes significant and prolonged.
Breaking the Cycle
Work with your pediatrician to identify specific triggers or patterns in your child’s infections.
Consider timing of infections — do they always follow colds, occur during certain seasons, or relate to other factors?
Track symptoms to help identify when infections are developing early, allowing for prompt treatment.
Maintain realistic expectations — some children will continue having ear infections despite best prevention efforts until they naturally outgrow the tendency.
The good news is that recurrent ear infections, while frustrating, are typically a temporary phase that improves as children grow and their ear anatomy matures.