When you have asthma, getting bronchitis isn’t just unpleasant—it can become dangerous quickly. Your already-sensitive airways react more severely to the inflammation and mucus that bronchitis causes. Understanding these added risks helps you recognize when you need immediate medical attention.
After treating asthma patients for three decades, I’ve learned to take bronchitis very seriously in this population.
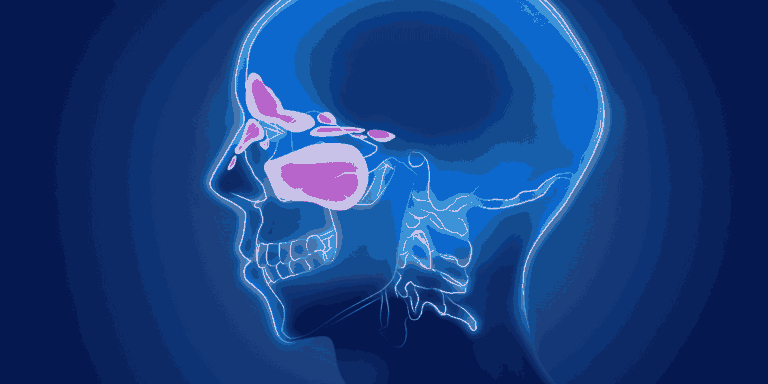
Why Asthma Makes Bronchitis Worse
Your airways are already prone to inflammation and narrowing with asthma. When bronchitis hits, it adds another layer of inflammation and fills your airways with mucus.
The combination can trigger severe asthma symptoms—wheezing, shortness of breath, chest tightness. What might be a mild illness in someone without asthma can land you in the emergency room.
Think of it like this: if your airways are already a narrow tunnel, adding inflammation and mucus turns them into a nearly blocked passage.
Symptoms Hit Harder and Faster
Most people with bronchitis develop a cough and feel crummy for a week. Asthma patients often experience rapid worsening of breathing within 24-48 hours.
You might notice increased use of your rescue inhaler, difficulty speaking in full sentences, or feeling winded doing normal activities. These are red flags that need immediate attention.
I had an asthma patient last year who developed bronchitis and waited three days before calling. By then she was using her inhaler every two hours and still struggling. We got her treated, but earlier intervention would have prevented that level of distress.
Increased Risk of Asthma Attacks
Respiratory infections like bronchitis are one of the most common triggers for asthma exacerbations. The infection irritates your already-hyperreactive airways, making them clamp down.
You might find your usual asthma medications aren’t controlling symptoms as well as they normally do. This isn’t a failure of your meds—it’s the added stress of infection on your system.
Longer Recovery Time
Asthma patients typically take longer to recover from bronchitis than people without asthma. Your airways need more time to calm down after the double hit of infection and asthma inflammation.
Even after the acute bronchitis resolves, you might have increased asthma symptoms for weeks. Your peak flow readings might stay lower than usual.
Treatment Requires Extra Attention
Through our telemedicine system, I ask specific questions to gauge how your asthma and bronchitis are interacting. Your treatment plan needs to address both conditions.
You’ll likely need to increase your controller inhaler temporarily. Some patients require oral steroids to get inflammation under control quickly.
Antibiotics only help if the bronchitis is bacterial, but we sometimes prescribe them more readily in asthma patients because the stakes are higher.
Warning Signs You Can’t Ignore
Difficulty speaking due to shortness of breath, using accessory muscles to breathe, rescue inhaler not providing relief, or peak flow dropping into the red zone—these all need emergency evaluation.
Bluish lips or fingernails mean you’re not getting enough oxygen. Call 911 immediately.
Prevention Strategies
Get your flu shot annually—influenza often leads to bronchitis. Consider the pneumonia vaccine based on your age and risk factors.
Keep your asthma well-controlled baseline. The better controlled it is before you get sick, the better you’ll handle infections.
At the first sign of bronchitis symptoms, contact your doctor. Early intervention prevents complications in asthma patients.