“It was just a small cut on my leg yesterday,” my patient said, pointing to an angry red area that had tripled in size overnight. “How did this happen so fast?”
Cellulitis can transform from a minor skin irritation to a medical emergency with frightening speed. Understanding why this happens — and recognizing early warning signs — can literally be lifesaving.
What Makes Cellulitis Different
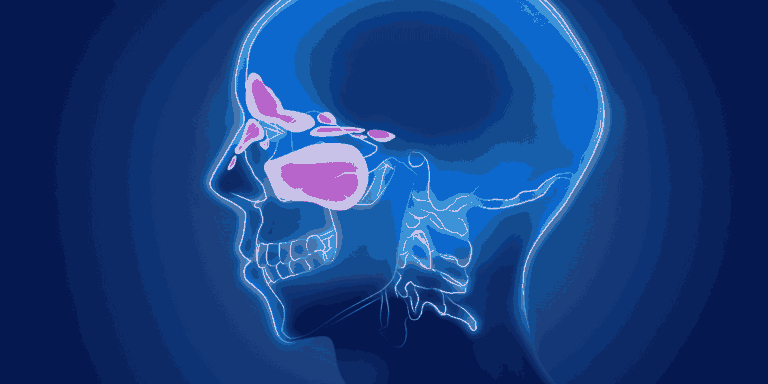
Unlike surface skin infections that stay localized, cellulitis affects deeper skin layers and subcutaneous tissue. The bacteria don’t just sit on top — they actively invade and spread through tissue planes.
Streptococcus and staphylococcus bacteria cause most cases, and both species produce enzymes that break down tissue barriers, allowing rapid spread.
Rich blood supply in deeper skin layers provides nutrients that fuel bacterial multiplication and transport infection throughout the body.
Why Speed Matters
Bacterial doubling time can be as short as 20-30 minutes under ideal conditions. What starts as a few bacteria can become millions within hours.
Tissue destruction occurs as bacteria release toxins that damage cells and blood vessels, creating more space for infection to spread.
Lymphatic involvement allows bacteria to travel through lymph vessels, spreading infection beyond the initial site.
Early Warning Signs
Rapid expansion of redness should alarm everyone. If you can draw around the red area and see it growing beyond those lines within hours, seek immediate care.
Increasing warmth indicates active infection and inflammation spreading through tissues.
Progressive pain that worsens quickly, especially if it seems disproportionate to the apparent injury.
Red streaking from the infected area toward the heart shows lymphatic spread — this requires emergency treatment.
Who Faces Higher Risk
Diabetes impairs immune function and circulation, making infections harder to control and more likely to spread rapidly.
Compromised immune systems from conditions like HIV, cancer treatment, or immunosuppressive medications can’t mount effective responses against bacterial invasion.
Poor circulation from heart disease, peripheral vascular disease, or prolonged inactivity reduces the body’s ability to deliver infection-fighting cells to affected areas.
Previous cellulitis episodes increase risk of recurrence, often in the same location where tissue damage may have occurred.
How Minor Injuries Lead to Major Problems
Any break in skin — cuts, scrapes, insect bites, or even tiny cracks from dry skin — provides bacteria entry points.
Common bacteria that normally live harmlessly on the skin’s surface become dangerous when they penetrate deeper layers.
Delayed treatment gives bacteria time to establish infection and begin spreading before the immune system can respond effectively.
Systemic Complications
Sepsis develops when bacteria enter the bloodstream and trigger body-wide inflammatory responses that can cause organ failure and death.
Necrotizing fasciitis represents the most severe form, where bacteria destroy fascia (tissue covering muscles), requiring emergency surgery.
Organ involvement can occur when bloodborne bacteria seed other body sites like heart valves, joints, or brain.
Why Antibiotics Must Start Quickly
Bacterial load increases exponentially with time. Early treatment faces fewer bacteria and has better success rates.
Tissue penetration becomes more difficult as infection progresses and local circulation becomes compromised.
Resistance development is more likely when treatment starts after bacteria have had time to multiply and potentially develop survival mechanisms.
Emergency Warning Signs
Seek immediate emergency care for:
- Fever with rapidly spreading skin infection
- Red streaks extending from infected area
- Severe pain that worsens quickly
- Signs of shock (rapid pulse, low blood pressure, confusion)
- Black or blue discoloration in infected areas
Treatment Urgency
Oral antibiotics work for early, mild cases but require close monitoring for progression.
IV antibiotics become necessary when infection shows signs of rapid spread or systemic involvement.
Hospitalization may be required for severe cases, elderly patients, or those with compromising conditions.
Surgery sometimes becomes necessary to remove dead tissue or drain infected collections.
Prevention Strategies
Wound care for even minor injuries prevents bacterial entry. Clean cuts promptly and keep them covered.
Skin maintenance includes moisturizing to prevent cracks and treating conditions like athlete’s foot that create skin breaks.
Hygiene practices reduce bacterial load on skin surface, decreasing infection risk when injuries occur.
Prompt attention to any signs of skin infection allows early intervention before serious complications develop.
The key message? Never underestimate seemingly minor skin infections. What appears minor can become life-threatening within hours. When in doubt, seek medical evaluation rather than waiting to see if things improve on their own.