A hiker found a tick on his arm after a weekend camping trip in Colorado. His friend, who found one after hiking in Connecticut, insisted they both needed antibiotics. But their Lyme disease risks were vastly different.
Understanding why some tick bites pose serious threats while others are essentially harmless can save you from unnecessary worry — or help you recognize when quick action is crucial.
Geographic Reality
Lyme disease doesn’t exist everywhere. The bacteria that cause it (Borrelia burgdorferi) only survives in specific tick species found geographic regions.
High-risk areas include the northeastern United States from Maine to Virginia, the upper Midwest (especially Wisconsin and Minnesota), and parts of northern California and Oregon.
Low-risk areas encompass most of the southern and western United States, where different tick species exist but don’t carry Lyme disease bacteria.
Tick Species Matters Enormously
Blacklegged ticks (also called deer ticks) in the Northeast and Midwest are the primary Lyme disease carriers. They’re tiny — adult females are about the size of a sesame seed.
Western blacklegged ticks on the Pacific Coast can also transmit Lyme disease, though infection rates are generally lower than eastern populations.
Other tick species like dog ticks, lone star ticks, or Rocky Mountain wood ticks don’t carry Lyme disease bacteria, regardless of where you encounter them.
Size and Life Stage Impact Risk
Nymph ticks (juvenile stage) pose the highest risk during late spring and summer. They’re incredibly small — about the size of a poppy seed — making them easy to miss.
Adult ticks are larger and easier to spot, typically active during cooler months in fall and early spring.
Larvae don’t carry disease because they haven’t had blood meals from infected animals yet.
Attachment Time is Critical
36-48 hour rule: Lyme disease transmission typically requires the tick to be attached for at least 36 hours. Ticks found and removed within 24 hours pose minimal infection risk.
Engorgement indicates duration. Flat ticks have been attached briefly, while engorged (swollen) ticks have been feeding longer and pose higher transmission risk.
Infection Rates in Tick Populations
Even in high-risk areas, not all ticks carry Lyme disease bacteria. Infection rates vary from 10-50% depending on specific location and tick population.
Local factors like deer populations, rodent density, and environmental conditions affect how many ticks in an area actually harbor the bacteria.
Recognition Challenges
Most people don’t remember being bitten because nymph ticks are so small and their bites are often painless.
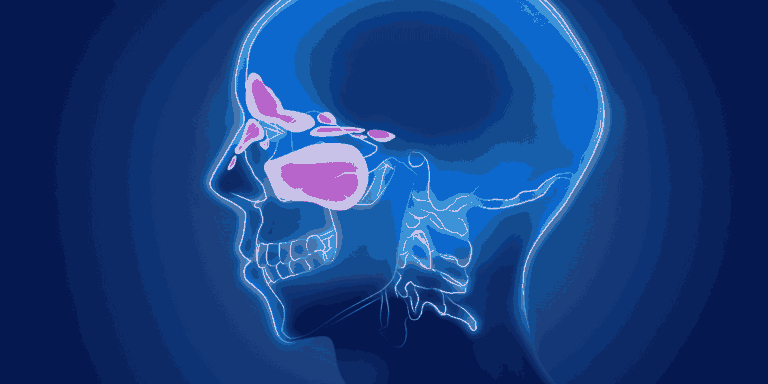
Tick attachment sites are frequently in hard-to-see areas like the scalp, armpits, or groin.
Rash development occurs in only 70-80% of Lyme disease cases, meaning you can’t rely on the classic “bull’s-eye” pattern for diagnosis.
When Prophylactic Antibiotics Make Sense
All criteria must be met:
- Tick identified as blacklegged tick species
- Attached for 36+ hours in high-risk geographic area
- Removed within 72 hours
- Treatment can start within 72 hours of removal
Single-dose doxycycline (200mg) effectively prevents Lyme disease when these criteria are met.
Other Tick-Borne Diseases
Rocky Mountain spotted fever occurs in different geographic areas and tick species than Lyme disease.
Ehrlichiosis and anaplasmosis can be transmitted by the same ticks that carry Lyme disease but require different evaluation approaches.
Southern tick-associated rash illness occurs with lone star tick bites but isn’t Lyme disease.
Risk Assessment Strategy
Document the details: Where were you when bitten? What did the tick look like? How long might it have been attached?
Consider the geography: Tick bites in most of Texas, Florida, or Arizona carry different risks than those in Massachusetts or Wisconsin.
Evaluate attachment time: Ticks found during daily checks pose less risk than those discovered after several days.
When to Worry vs. When to Watch
Immediate concern: Tick bite in high-risk area with confirmed long attachment time.
Watchful waiting: Most other tick bite situations where monitoring for symptoms over 30 days is appropriate.
No concern: Tick bites from non-Lyme-carrying species or outside endemic areas.
Monitoring for Symptoms
Expanding rash that develops 3-30 days after tick bite, especially if it resembles a target or bull’s-eye pattern.
Flu-like symptoms including fever, headache, and muscle aches appearing days to weeks after tick removal.
Joint pain or neurological symptoms that develop weeks to months later in untreated cases.
Understanding that tick bite risks depend on specific circumstances — geography, tick species, attachment time, and individual factors — helps you make informed decisions about whether prophylactic treatment or watchful monitoring is most appropriate for your situation.