“My daughter’s been coughing for three weeks,” a frustrated mother told me during our virtual consultation. “She doesn’t seem that sick, but this cough won’t go away.”
Walking pneumonia gets its name because kids often don’t look or feel as sick as you’d expect with a lung infection. But that persistent, nagging cough is your first clue something more serious might be brewing.
What Makes Walking Pneumonia Different
Mycoplasma pneumonia causes most walking pneumonia cases in children. Unlike typical pneumonia bacteria, mycoplasma creates milder but more persistent symptoms.
Gradual onset means symptoms develop slowly over days to weeks, rather than the sudden illness typical of bacterial pneumonia.
Less severe appearance allows children to maintain relatively normal activity levels despite having a lung infection.
The Telltale Cough Pattern
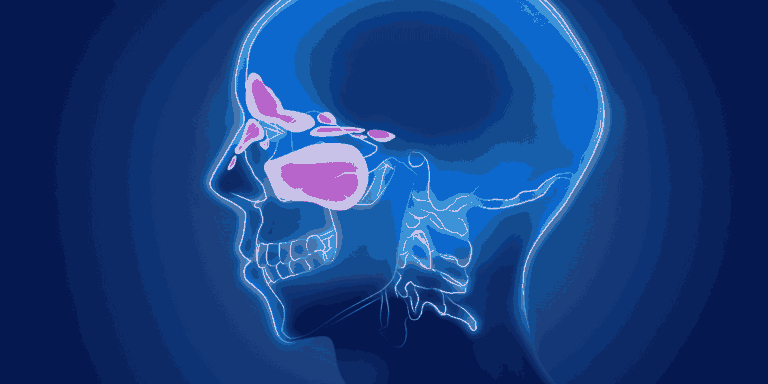
Persistent dry cough that lasts weeks, not days, is walking pneumonia’s calling card. This isn’t the productive, mucus-filled cough of typical chest colds.
Worse at night — the cough often intensifies when children lie down, disrupting sleep for the whole family.
Doesn’t respond to typical cough suppressants or cold medications that usually provide some relief.
Progressive nature means the cough may actually get worse over time rather than improving like normal respiratory infections.
Age-Specific Patterns
School-age children (5-15 years) develop walking pneumonia most frequently. Younger children and toddlers can get it but less commonly.
Adolescents often experience more severe symptoms including significant fatigue and prolonged recovery periods.
Preschoolers may have more subtle symptoms, making diagnosis challenging for parents and healthcare providers.
Associated Symptoms to Monitor
Low-grade fever that comes and goes, rather than high persistent fevers seen with typical pneumonia.
Fatigue that seems disproportionate to other symptoms — children may seem unusually tired or lack their normal energy.
Headaches and general feeling of being unwell, similar to having the flu but lasting much longer.
Sore throat sometimes accompanies the cough, leading parents to initially suspect strep throat or viral infections.
When to Suspect Walking Pneumonia
Duration matters most — coughs lasting more than 2-3 weeks, especially if they’re not improving or getting worse.
School outbreaks are common because mycoplasma spreads easily in close-contact environments like classrooms.
Family clusters may develop when one child brings the infection home and spreads it to siblings over several weeks.
Diagnosis Challenges
Normal chest X-rays can occur early in the illness, making diagnosis difficult based on imaging alone.
Physical examination may reveal subtle lung sounds that suggest infection, but children often don’t appear seriously ill.
Blood tests can help identify mycoplasma infection, though results may take several days.
Why Early Recognition Matters
Antibiotic response is excellent when walking pneumonia is identified and treated appropriately with macrolide antibiotics like azithromycin.
Symptom duration shortens significantly with proper treatment compared to letting the infection run its course.
Spread prevention helps protect family members and classmates from developing the same persistent illness.
Treatment Expectations
Improvement timing — children typically feel better within 2-3 days of starting appropriate antibiotics, though complete cough resolution may take 1-2 weeks.
Activity restrictions are usually minimal, but strenuous exercise should be avoided until symptoms resolve.
Return to school can often happen once fever resolves and children feel well enough to participate normally.
Red Flags for Complications
Seek immediate care if your child develops:
- High fever (over 102°F) with the persistent cough
- Difficulty breathing or rapid breathing
- Chest pain that worsens with deep breathing
- Signs of dehydration or inability to eat/drink normally
The bottom line: Don’t ignore persistent coughs lasting more than 2-3 weeks in school-age children. Walking pneumonia is highly treatable once identified, but the key is recognizing that a “minor” cough can indicate a significant lung infection requiring antibiotic treatment.