Women are significantly more prone to UTIs, experiencing them at a rate 8-10 times higher than men. This striking difference isn’t due to hygiene habits or behavior—it’s primarily anatomical.
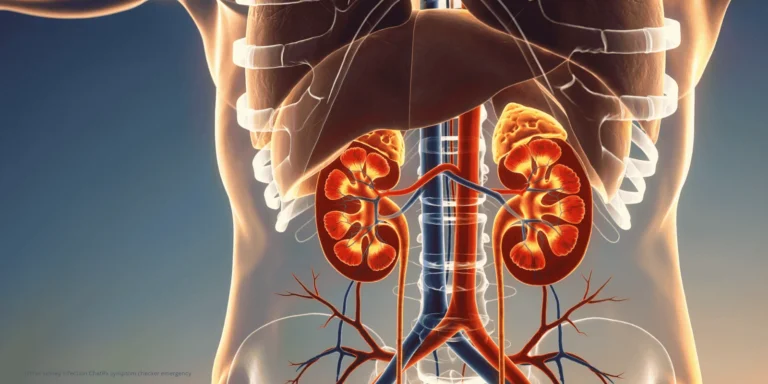
The female urethra is much shorter than the male urethra—only about 1.5 inches compared to 8 inches in men. This shorter distance gives bacteria a much easier pathway to reach the bladder. Think of it as the difference between climbing a single flight of stairs versus climbing eight flights—bacteria find the shorter route far more manageable.
Additionally, in women, the urethral opening is located closer to the anal area, where E. coli bacteria naturally reside. This proximity increases the likelihood of bacterial transfer, especially during activities like wiping, sexual intercourse, or general daily movement.
Hormonal factors also play a role. Estrogen helps maintain the acidic pH and healthy bacterial balance in the urogenital area. During menopause, declining estrogen levels can alter this protective environment, making post-menopausal women even more susceptible to UTIs.
Sexual activity affects women disproportionately due to anatomy. During intercourse, bacteria can be pushed toward the urethral opening and into the bladder more easily in women than men. This is why “honeymoon cystitis”—UTIs in newly sexually active women—is a recognized phenomenon.
Men do get UTIs, but they’re often associated with:
- Prostate problems that obstruct urine flow
- Kidney stones
- Catheter use
- Underlying health conditions
Pregnancy creates additional UTI risk for women due to hormonal changes, urinary tract structure modifications, and the growing uterus potentially obstructing complete bladder emptying.
Understanding these anatomical and physiological differences helps explain why prevention strategies often focus on women and why UTIs in men warrant closer medical evaluation.
If you’re experiencing frequent UTIs, ChatRx can help determine appropriate treatment and discuss prevention strategies tailored to your specific situation.