“My ear hurts, but I don’t have any drainage or fever,” my patient explained. “Does that mean it’s not infected?”
Ear pain and ear infections aren’t always the same thing. Understanding the differences helps determine when medical treatment is necessary versus when simpler measures will suffice.
Types of Ear Pain Without Infection
TMJ disorders create ear pain that worsens with jaw movement, chewing, or teeth clenching.
Dental problems like cavities or abscesses refer pain to the ear through shared nerve pathways.
Sinus pressure from allergies or congestion can cause ear fullness and discomfort without infection.
Earwax buildup creates pressure and pain but doesn’t involve bacterial or viral infection.
Eustachian tube dysfunction causes ear pressure changes during altitude shifts or colds without actual infection.
True Ear Infection Characteristics
Fluid drainage from the ear, especially if colored or foul-smelling, strongly suggests infection.
Fever accompanying ear pain indicates inflammatory response to bacterial or viral infection.
Hearing loss or muffled hearing occurs when infection creates fluid buildup behind the eardrum.
Severe, throbbing pain that worsens at night is characteristic of middle ear infections.
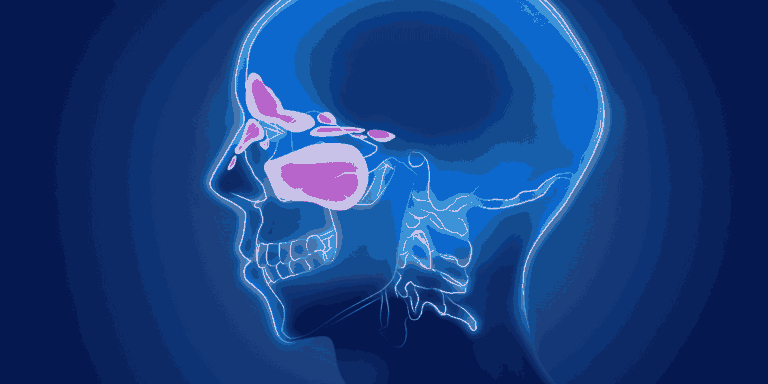
Location Matters Significantly
Middle ear infections (otitis media) occur behind the eardrum and typically follow colds or allergies.
Outer ear infections (swimmer’s ear) affect the ear canal and hurt worse when the outer ear is pulled or pressed.
Pain location helps distinguish infection types — deep, internal pain versus pain in the visible ear canal.
Associated Symptoms
Recent cold symptoms followed by ear pain suggest secondary middle ear infection development.
Water exposure before ear pain onset points toward swimmer’s ear rather than middle ear infection.
Nasal congestion often accompanies middle ear infections due to connected eustachian tubes.
Balance problems or dizziness can indicate inner ear involvement beyond simple infection.
Age-Related Patterns
Children more commonly develop middle ear infections due to immature eustachian tube structure.
Adults experiencing ear pain often have external causes like TMJ, dental issues, or swimmer’s ear rather than middle ear infections.
Elderly patients may have ear pain from nerve problems or shingles affecting the ear area.
Duration Considerations
Sudden onset severe pain with fever suggests acute bacterial infection requiring antibiotics.
Gradual development over days with cold symptoms might represent viral infection or eustachian tube dysfunction.
Chronic intermittent pain suggests non-infectious causes like TMJ, dental problems, or referred pain.
Pain Patterns That Guide Diagnosis
Pain with ear manipulation — pulling the outer ear or pressing the tragus causes severe pain with swimmer’s ear but not middle ear infections.
Position-related changes — pain worsening when lying down suggests middle ear infection, while pain unaffected by position points to other causes.
Chewing-related pain indicates TMJ or dental problems rather than ear infection.
When Antibiotics Are Needed
Bacterial ear infections require antibiotic treatment to prevent complications and speed recovery.
Viral infections resolve without antibiotics, though pain management remains important.
Non-infectious causes need treatment addressing the underlying problem rather than antibiotics.
Home Assessment Tips
Pull test — gently pull the outer ear upward and outward. If this causes significant pain, swimmer’s ear is likely.
Pressure test — press on the small bump in front of the ear canal opening. Pain with this suggests external ear infection.
Movement test — chew or move your jaw. If pain worsens, TMJ or dental problems are more likely than ear infection.
Red Flags for Serious Problems
Severe headache with ear pain may indicate spreading infection or complications.
Facial weakness on the side of ear pain suggests nerve involvement requiring immediate attention.
High fever (over 102°F) with ear pain needs medical evaluation for appropriate treatment.
Persistent drainage or blood from the ear warrants urgent assessment.
When Medical Evaluation Is Needed
Pain lasting more than 2-3 days without improvement suggests need for professional diagnosis.
Hearing loss accompanying ear pain requires examination to prevent permanent damage.
Recurring episodes indicate underlying problems that need identification and treatment.
Uncertainty about cause — when in doubt, professional evaluation ensures proper treatment and prevents complications.
Self-Care Limitations
Over-the-counter pain relievers help manage discomfort but don’t treat underlying infections.
Warm compresses provide temporary relief but won’t cure infections requiring antibiotics.
Attempting self-diagnosis risks delayed treatment of serious conditions requiring specific interventions.
Understanding the distinction between ear pain and ear infection helps you make informed decisions about when home care is sufficient versus when medical attention is necessary.