“I got the flu shot last year,” my patient said. “Why do I need another one already?”
Influenza’s unique ability to constantly change makes annual vaccination necessary. Understanding why flu viruses evolve so rapidly helps explain this yearly ritual that frustrates many people.
How Influenza Mutates
Antigenic drift occurs when small genetic changes accumulate in flu viruses over time, creating slightly different strains each season.
Random mutations during viral replication happen naturally, with some changes allowing the virus to evade previous immune responses.
Selection pressure from human immunity drives evolution — viruses that successfully bypass existing antibodies spread more effectively.
Two main types (Influenza A and B) circulate simultaneously, each capable of independent genetic changes.
Why Last Year’s Vaccine Doesn’t Work
Antibody mismatch develops when circulating flu strains differ enough from vaccine strains that immune protection fails.
Waning immunity means antibody levels decline over months, reducing protection even against similar strains.
New genetic combinations emerge when multiple flu strains infect the same host, swapping genetic material.
The Prediction Challenge
Six months ahead — vaccine composition decisions happen before flu season begins, requiring educated guessing about future strains.
Global surveillance tracks circulating flu variants worldwide to inform vaccine strain selection.
Sometimes predictions miss — when vaccine strains don’t match circulating viruses, effectiveness decreases significantly.
Multiple strains included — most flu vaccines protect against 3-4 different flu strains simultaneously.
Geographic Variations
Southern hemisphere data helps predict northern hemisphere flu season since their winter precedes ours.
Strain dominance shifts — the primary flu strain causing illness can change mid-season.
International travel spreads flu variants globally, introducing new strains to different regions.
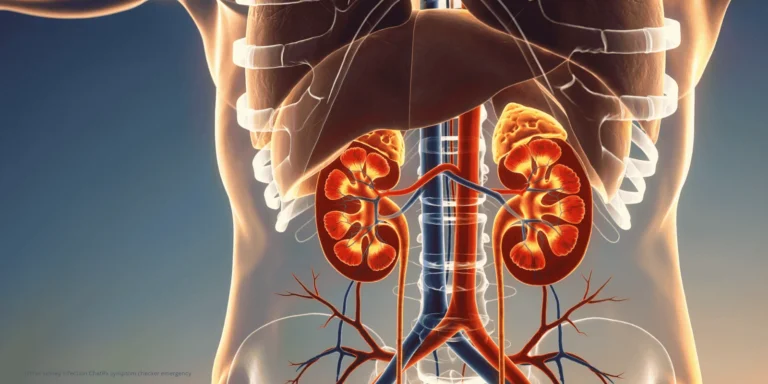
Animal Reservoirs Complicate Matters
Bird flu viruses occasionally jump to humans, creating completely new strains against which populations have no immunity.
Pig infections allow genetic mixing between human, bird, and pig flu viruses, potentially creating pandemic strains.
Constant evolution in animal populations creates endless sources of new flu variants.
Why We Can’t Make One Permanent Vaccine
Surface protein changes (hemagglutinin and neuraminidase) alter the targets that antibodies recognize and attack.
Rapid mutation rate outpaces slower evolutionary changes in other viruses that allow long-term immunity.
Multiple viral lineages circulate simultaneously, each evolving independently.
Vaccine Development Timeline
February decision for northern hemisphere vaccines, based on southern hemisphere flu season data.
Manufacturing process takes 6 months, requiring early commitment to specific strains.
Distribution begins in late summer for fall vaccination campaigns.
Effectiveness Variations
Good match years see 40-60% effectiveness at preventing illness.
Poor match years still provide 10-30% protection and reduce severity in breakthrough cases.
Age factors affect response — elderly and very young develop weaker immunity from vaccination.
Partial Protection Benefits
Reduced severity occurs even when vaccines don’t prevent infection entirely.
Lower hospitalization rates among vaccinated people who do get flu.
Decreased transmission helps protect vulnerable populations who can’t be vaccinated.
Future Vaccine Technologies
Universal flu vaccines targeting unchanging viral components are in development.
mRNA platforms like those used for COVID vaccines may allow faster seasonal updates.
Broader protection approaches aim to combat multiple flu strains with single vaccines.
Why Annual Vaccination Remains Important
New strains circulate each year requiring updated immune responses.
Community protection reduces overall flu transmission when vaccination rates are high.
Vulnerable populations benefit from “herd immunity” created by widespread vaccination.
Best available tool — despite imperfections, annual flu vaccination remains our most effective flu prevention strategy.
The constant genetic changes in influenza viruses mean we’re always playing catch-up, requiring annual vaccine updates to maintain population protection against evolving threats.